In This Issue
No Goodbyes on the Doorstep: Bear Clan Patrol Ensures Safety of Woman with Dementia
How to Make Your Spiritual Community More Dementia Friendly: Part 2 of a Two-part Series
Understanding Changes in Eating Patterns Among People with Dementia
Lifestyle Changes Could Prevent a Third of Dementia Cases
Education and Programs
Events and Volunteering
No Goodbyes on the Doorstep:
Bear Clan Patrol Ensures Safety of Woman with Dementia
 Four female members of Winnipeg’s Bear Clan Patrol were nearing the end of their evening shift on a cold, slippery night last March when a man hailed them. Concerned about an elderly woman he had found wandering on the street, the man asked the Bear Clan volunteers – Cara, Krista, Susan and Patty – to assist.
Four female members of Winnipeg’s Bear Clan Patrol were nearing the end of their evening shift on a cold, slippery night last March when a man hailed them. Concerned about an elderly woman he had found wandering on the street, the man asked the Bear Clan volunteers – Cara, Krista, Susan and Patty – to assist.
The woman seemed frail, lost and disoriented and was not dressed for the cold weather. Using a bit of detective work, the Bear Clan members discovered her address; they drove her to her home and escorted her inside.
But that is not the end of this story.
“Even though she was safe for the moment, we felt she displayed signs of dementia, and we were really concerned,” explains Cara, who also works in the Administration Department at the Alzheimer Society of Manitoba. “We wanted to contact a family member or friend who would be able to check in on her later.”
Krista called a phone number that was posted on the wall in the woman’s home. Herlenda Bermejo-Basas of Burnaby, British Columbia, answered. It turns out that Herlenda is the sister of the woman, whose name is Pilar. 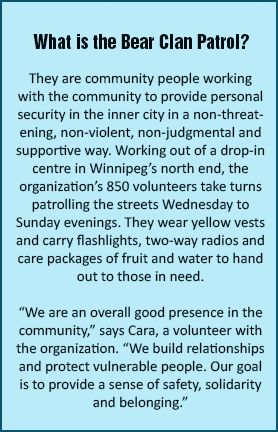
By not saying goodbye to Pilar at her doorstep, these four Bear Clan volunteers acted in the spirit of a dementia friendly community. By taking the time to make that call, Pilar’s family was alerted to her circumstances. Soon after, they made arrangements for Pilar to move into a care facility in Burnaby close to Herlenda’s home.
High Priority
Encouraging communities to be dementia friendly is a high priority for the Alzheimer Society, and CEO Wendy Schettler views the story of Pilar and the Bear Clan Patrol as a prime example for others to follow.
“A dementia friendly community is one that encourages individuals and organizations to be leaders when it comes to including people with dementia and offering to assist if someone needs help,” she says. “This group of Bear Clan volunteers did just that, and took it one step further by ensuring the future safety of a person with dementia.”
Pilar’s family is appreciative of the actions of Cara, Krista, Susan and Patty on that cold March night in Winnipeg’s north end. “Please accept our gratitude,” says Herlenda. “We will always remember the Bear Clan Patrol of Winnipeg.”
How to Make Your Spiritual Community More Dementia Friendly
Part 2 of a Two-part Series
 In our August eNewsletter, we presented ways that worship centres can be supportive and inclusive of people with dementia. In this issue, we’d like to discuss how spiritual communities – regardless of the beliefs observed – can also support family and friends who are caring for a person with dementia.
In our August eNewsletter, we presented ways that worship centres can be supportive and inclusive of people with dementia. In this issue, we’d like to discuss how spiritual communities – regardless of the beliefs observed – can also support family and friends who are caring for a person with dementia.
The first step towards accomplishing this important mission is to ask the care partner how you can help. If the person does not have a ready suggestion, don’t forget to ask again as their needs change over time. Remember: as the family member’s dementia progresses, help may be needed and will be appreciated.
Here are some ways that a spiritual community can reach out to care partners:
- If care partners have not been able to attend services, they are still part of the spiritual community. Reach out to them by phone, email or text to let them know you care.
- When care partners are able to attend church with the person with dementia, don’t crowd them; this may make the person uncomfortable. Do include the person with dementia in the conversation as you talk to their care partner.
- If the person with dementia and their care partner have missed a number of gatherings, don’t comment on their absence. Instead, celebrate their attendance today.
- Consider visiting with the person with dementia one-on-one in a quieter space so the care partner can have a few minutes to engage with other friends.
- Check in with the care partner before dropping in for a visit at their home. If they tell you that today is not a good day, respect their wishes.
- If a person is caring for someone at a distance and you know they are finding their support role emotionally stressful, remember to support that person with kind words or actions – just as you would if they were caring for someone in their home or community on a daily basis.
Support given by members of the congregation at your church, synagogue, mosque or temple is of great value to people with dementia and their care partners. Consider these and other strategies that your place of worship could adopt to become dementia friendly.
The Alzheimer Society can help any community group become more dementia friendly. You can arrange for a dementia friendly community presentation by calling us at 204-943-6622 or by emailing [email protected]
Understanding Changes in Eating Patterns Among People with Dementia
 Regular eating habits and proper nutrition help maintain a person’s health and well-being. Dementia, along with other physical and sensory changes, can affect eating patterns and the person’s ability to maintain good nutrition.
Regular eating habits and proper nutrition help maintain a person’s health and well-being. Dementia, along with other physical and sensory changes, can affect eating patterns and the person’s ability to maintain good nutrition.
It is important to understand the reason for a change in habits, although this can be difficult, particularly if the person is struggling to find the words to explain it. The following are some reasons why the person may not be eating well and ways to help:
- Forgetting to eat or that they have already eaten: Have visual cues or reminders to orient the person to mealtimes. A reminder message on an electronic device or a clearly visible note posted on the fridge may help.
- Change in ability to recognize food or drink or how food is presented: Orient the person to what is being served and present the food in familiar ways i.e. scoop ice cream on top of the pie if that’s how the person used to enjoy it.
- Changes in senses of smell and taste: Include more flavourful spices, herbs and vegetables. Use aromatic techniques (i.e. slow cooking, simmering, baking) to create more flavorful dishes while producing mouth-watering aromas.
- Vision changes: Use colorful foods; separate each part of the meal so foods are clearly seen on the plate; serve meals on dishes that contrast with the color of the foods being served.
- Changes in oral health: Serve soft, moist food cut into smaller pieces; opt for fish or ground meat rather than whole cuts; serve meals with healthy sauces to help moisten food and facilitate chewing and swallowing.
- Feelings of fullness because of constipation: Encourage the person to increase their fiber and fluid intake and to engage in physical activity as often as they are able.
- Medications: Consult the person’s doctor or pharmacist if any of the medications taken affect appetite or cause constipation, nausea, vomiting, diarrhea, bad tastes in the mouth or dry mouth. The doctor may be able to make changes in the dosage or the time of day when medication is taken to avoid these effects.
It is also important to consult with the person’s doctor when there are changes in appetite or eating habits. Remember that mealtimes are enjoyed most when they are shared with others. Plan to make mealtimes a relaxed activity that you will enjoy together.
Lifestyle Changes Could Prevent a Third of Dementia Cases
 Research indicates that lifestyle factors have a strong impact on your risk of developing dementia. More than a third of dementia cases might be avoided by tackling aspects of lifestyle, including education, exercise, blood pressure and hearing, suggests a Lancet report released July 2017. These lifestyle changes should begin early and continue through the life span.
Research indicates that lifestyle factors have a strong impact on your risk of developing dementia. More than a third of dementia cases might be avoided by tackling aspects of lifestyle, including education, exercise, blood pressure and hearing, suggests a Lancet report released July 2017. These lifestyle changes should begin early and continue through the life span.
Major risk factors identified at different life stages are:
- In early life: Less time in education increases vulnerability to cognitive decline because of potentially less cognitive reserve.
- In midlife: Hearing loss, hypertension and obesity have been shown to impact cognitive decline.
- In late life: Smoking, depression, physical inactivity, social isolation and diabetes have been identified as factors that could increase an individual’s risk of dementia.
These factors make up about 35 percent of the overall risk of developing dementia; the remainder can be attributed to non-modifiable factors such as aging, genetics and family history. Taking preventative action to reduce your risk may push back the onset of dementia for many years, giving more quality time to enjoy with family and friends.
Watch for subsequent research articles that will discuss ways to reduce your risks.
Education and Programs
